Point solutions. For HR and benefit teams, that was the buzz-term of 2022.
In the past, self-funded employers managed healthcare costs by pursuing the best discounts and widest networks with their health plan partners. But, as our conversations this year with dozens of HR and benefits leaders made clear, the tide is turning.
With costs constantly rising—often without a corresponding boost in outcomes—there is increasing pressure on employers to play a more proactive role in selecting benefit programs that deliver real value.
Here are our three year-end trends for HR and benefit leaders:
1. Point solution programs are all the rage! But how to choose?
There was a lot of uncertainty this year for employers, from the lingering effects of the pandemic and the “Great Resignation” to rising interest rates and recession fears.
The labor shortage combined with ever-rising healthcare costs has convinced many employers to be more strategic in designing an overall benefits package to attract and retain top talent while also meeting the unique needs of their existing employees.
This means selecting point solution programs that will have a real impact on health, well-being, and productivity. But the first challenge many employers face when trying to be more proactive is that they’re overwhelmed with options—from disease management programs to digital wellness apps to fitness trackers and more.
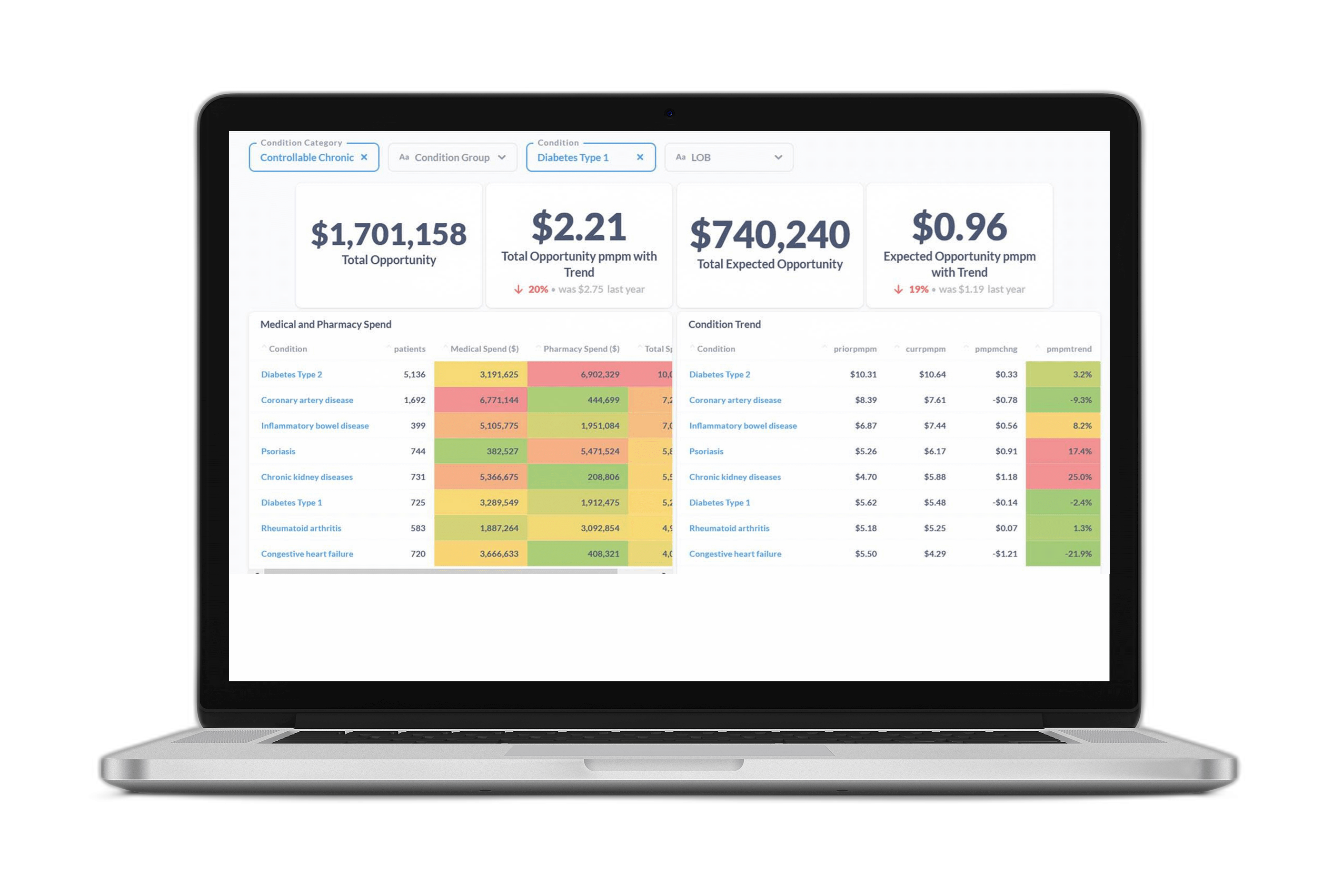
To cut through the noise, many employers are turning to predictive insights to help them make smarter, faster decisions.
2. Connecting your data is the first step to more proactive benefit design
“Predictive analytics.” “Machine learning.” “AI.”
These can be intimidating terms for HR and benefits professionals. And yet, over the past year we’ve seen more and more large employers seeking to optimize their benefit plans and attract the workforce of the future using predictive insights.
These companies generate large amounts of benefits data—including medical, pharmacy, disability, and worker’s comp claims, plus program enrollment and engagement metrics and more—that can be used to make better decisions when designing a benefits plan. But first it all has to be connected, cleansed, standardized, enriched, and validated.
Increasingly, employers are contracting with data warehouse vendors to unify and add power to their data. The benefits of working with an experienced data warehousing vendor include having all data in one place, being able to share insights with partners and vendors, and uncovering hidden savings opportunities to ensure healthcare dollars are being spent as wisely as possible.
3. With a data strategy in place, you can select the best point solutions for your employees
We spoke to many HR and benefits teams this year who listed a number of questions they’re trying to answer as they seek to improve their benefit offerings. These include:
- Should they invest in diabetes management, heart health, fitness tracking, clinical outreach, mental health services, or an array of other choices?
- How can they get employees and their families to engage with each program to its fullest potential?
- How can they measure the success of these programs?
Answering these questions requires a data-backed approach to understanding the specific needs of an employer population and quantifying the impact of new and existing programs. Over the past year at Certilytics, we’ve helped customers answer these questions using our Impact Evaluator, which equips HR and benefits teams with easy-to-understand insights into which point solutions are the right fit to achieve their goals.
Our program evaluation tool enables employers to quantify the impact of new and existing point solution programs, boost employee engagement, and measure performance to ensure ROI.
To learn more about how Certilytics can help you connect your data and make smarter benefit decisions, contact us to schedule a meeting with our team.