Certilytics was thrilled to be a first-time exhibitor at this year’s HIMSS conference, and we’re delighted so many people made time to stop by our booth and attend our receptions.
Attendance overall may have been down due to the COVID-19 Delta variant, but there was enormous pent-up energy from those who attended to meet with old friends and make new connections—with masks on and hands sanitized.
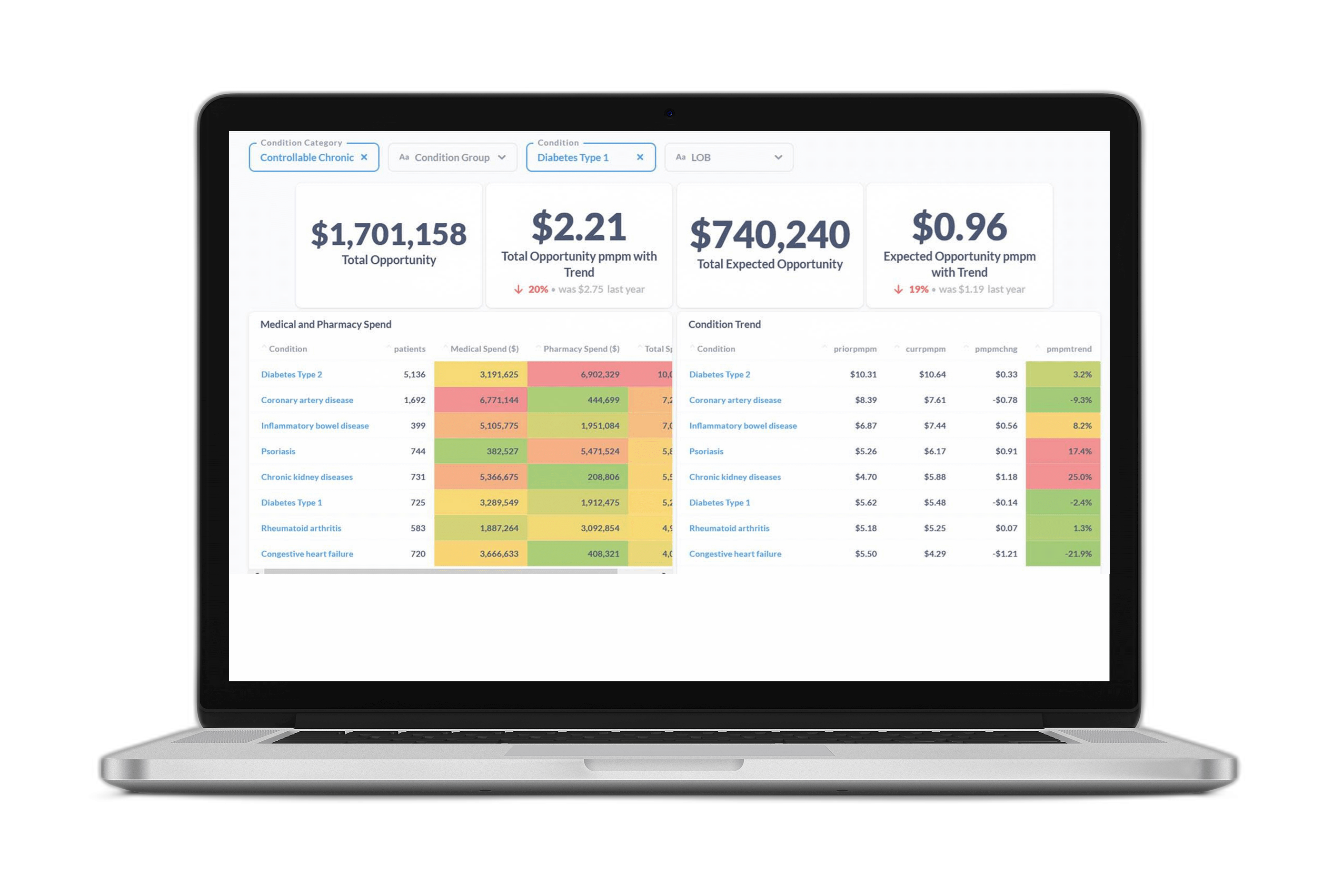
At our booth, HIMSS attendees calculated more than $1.4 billion in total financial opportunity and avoidable overspending using our web-based $PMPM Savings Calculator, which demonstrates the power of predictive analytics to unlock value.
Here are five things we learned from an unforgettable conference:
The Digital Health Revolution Has Arrived
Digital health and virtual care have been major buzzwords at past conferences, but the pandemic has brought them to the forefront—and there’s no turning back.
Increasingly, healthcare organizations and self-insured employers will be seeking to improve population health and realize value through digital tools and outreach methods. This will require strategic investments in data analytics that support reaching the right patients at the right time via the right form of outreach—a key capability we help our clients achieve through our risk stratification tool.
The pandemic is also accelerating the shift toward virtual care and telehealth, which will require investment in AI capabilities that ensure individual patients are matched with the right services and care settings. That’s why Certilytics built a predictive model that determines a patient’s likelihood of utilizing telehealth services—enabling our clients to target their virtual care programs more effectively.
Reporting Tools Should Look Forward, Not Backward
In the past, many healthcare organizations focused on retrospective utilization rates when deciding which members to prioritize for medical management. But, as several HIMSS panels made clear, this approach was built to serve an outdated fee-for-service model, not value-based care arrangements—and it ignores the fact that the highest-cost members aren’t always the ones who will benefit most from clinical intervention. A member with lower overall predicted financial risk—but more open care gaps or redirection opportunities—might be a better candidate for outreach, especially if the member shows a high propensity for engagement.
As healthcare organizations transition to value-based care, they’re moving toward prospective reporting that predicts not just risk, but modifiable risk, as we do through the Certilytics Opportunity Framework. This is the best way to reach members before they incur avoidable, exorbitant costs—and unlock true value while improving population health.
Healthcare Leaders Want Access to Their Data
It was a major theme at the conference: Healthcare organizations want to be able to access their connected data and build their own visualizations to serve their specific business or clinical needs.
Many of the leaders we met during HIMSS21 seemed to have a shared vision for what they’re looking for. They want a self-service business intelligence tool that can empower their teams to make rapid, data-driven decisions, and easily share population- and patient-level insights. Intuitive, interactive data exploration and visualization capabilities are a must-have, as is the ability to easily create custom reports.
We were thrilled to be able to share how our Healthcare Data & Prediction Platform meets those mission-critical needs and gives clinical and financial teams direct access to their cleansed, standardized, and enriched source data.
Data Must be Integrated Across Benefits
Fully connecting medical and pharmacy data was another common theme in many of the conversations we had at the conference. There was clearly frustration with traditional data warehouse vendors’ offerings when it comes to integrated, cross-benefit analysis. Again and again, leaders spoke about the need to answer foundational questions, like how intervention on one benefit (such as drug compliance) impacts other benefits (like medical utilization and avoidance of the ER).
With the CORE® clinical episode grouper, Certilytics integrates pharmacy and medical data to form a complete picture of member health, connecting the dots and quantifying the impact of each activity on a patient’s total healthcare costs.
Reining in Specialty Rx Costs is a Major Priority
Specialty pharmacy spending seemed to be on everyone’s minds in one way or another—from how specialty drugs are transforming patients’ lives to how home infusion is impacting outpatient care pathways to which novel drugs in the FDA pipeline hold new promise for treating rare diseases.
No matter the area of focus, questions related to cost almost always came up. How can employers and health plans get a handle on specialty drug spending? How can organizations streamline and improve decision-making related to care setting (outpatient, inpatient, or the home) so that the drug is administered in the setting most likely to produce the best outcome? And what strategies are most effective at reining in costs and protecting against catastrophic claims?
It was inspiring to hear so many leaders talk about their commitment to finding new ways to work with their partners across healthcare to answer these questions so that all patients can have access to the therapies they need.
Thanks again to all those who made time to connect with us in Las Vegas—we hope to connect again (or for the first time) at HIMSS22 in Orlando!
For a free consultation with our team of experts, reach out to us at contact@certilytics.com