As HLTH 2021 wraps up, Certilytics would like to thank everyone who made time to connect with us—whether at a pre-scheduled meeting, at our reception, or just bumping into one of our team members at an event or panel session.
Here are Five Things we Heard and Learned at this Year’s Conference
1. It’s All About Data Connectedness
A quick stroll through the exhibit hall made clear the large number of exhibitors promoting health and wellness apps, each of which collects data that could inform better strategies for improving population health and managing total cost of care.
But as one executive put it, it’s not about getting access to more data—it’s about connecting the data you already have.
The most successful data warehousing and predictive analytics vendors are those that have proven the ability to connect a wide variety of data sources, including integrating medical and pharmacy data, to build patient risk profiles that encapsulate the full range of available information.
2. Social Determinants of Health is More Than a Buzzword
For years now, healthcare leaders have been talking about health equity and the Social Determinants of Health (SDOH). But these concepts have often felt like buzzwords, with few ideas for how to respond to the growing understanding that factors outside a clinician’s control have a major impact on health.
But at HLTH 2021, healthcare leaders from across the spectrum were sharing stories of how they’re beginning to turn this knowledge into real-world action.
At Certilytics, we recently released an AI-powered model that predicts each patient’s SDOH risk, enabling interventions at both the member and population levels to improve healthcare access and outcomes with cost and efficiency measures.
This model is designed to help health plans, employers, and provider health systems gain deeper insights into member behaviors and develop new strategies, programs, and partnerships to address social health barriers.
3. The Pandemic is Powering a Digital Health Revolution
The COVID-19 pandemic has brought digital health to the forefront—and there’s no turning back.
As the panel sessions made clear, healthcare organizations and employers will increasingly be seeking to improve population health and realize and enhance their value through digital tools and outreach methods. This will require strategic investments in data analytics that support reaching the right patients at the right time via the right form of outreach—a key capability we help our clients achieve through our risk stratification tool.
The pandemic is also accelerating the shift toward virtual care and telehealth, which will require investment in AI capabilities that ensure individual patients are matched with the right services and care settings. That’s why Certilytics built a predictive model that determines a patient’s likelihood of utilizing telehealth services—enabling our clients to target their virtual care programs more effectively.
4. Specialty Rx costs are a Major Concern
At the conference, rising specialty pharmacy costs were a major focus for payer organizations. And for good reason: Plan sponsors are seeing more and more of their total pharmacy spend being attributed to specialty drugs. Evernorth’s 2020 Drug Trend Report found that just 2% of the company’s covered population used specialty drugs—but this accounted for over half of total spend under the pharmacy benefit.
5. The Industry has Fully Embraced Value-Based Care
Conversations with leaders at HLTH made it clear: The industry is fully committed to transitioning from an outdated fee-for-service model to value-based care.
This is driving a major shift in population health management, as well.
In the past, many healthcare organizations focused on retrospective utilization rates when deciding which members to prioritize for medical management. But this approach was built to serve the fee-for-service model—and it ignores the fact that the highest-cost members aren’t always the ones who will benefit most from clinical intervention. A member with lower overall financial risk—but more open care gaps or redirection opportunities—might be a better candidate for outreach, especially if the member shows a high propensity for engagement.
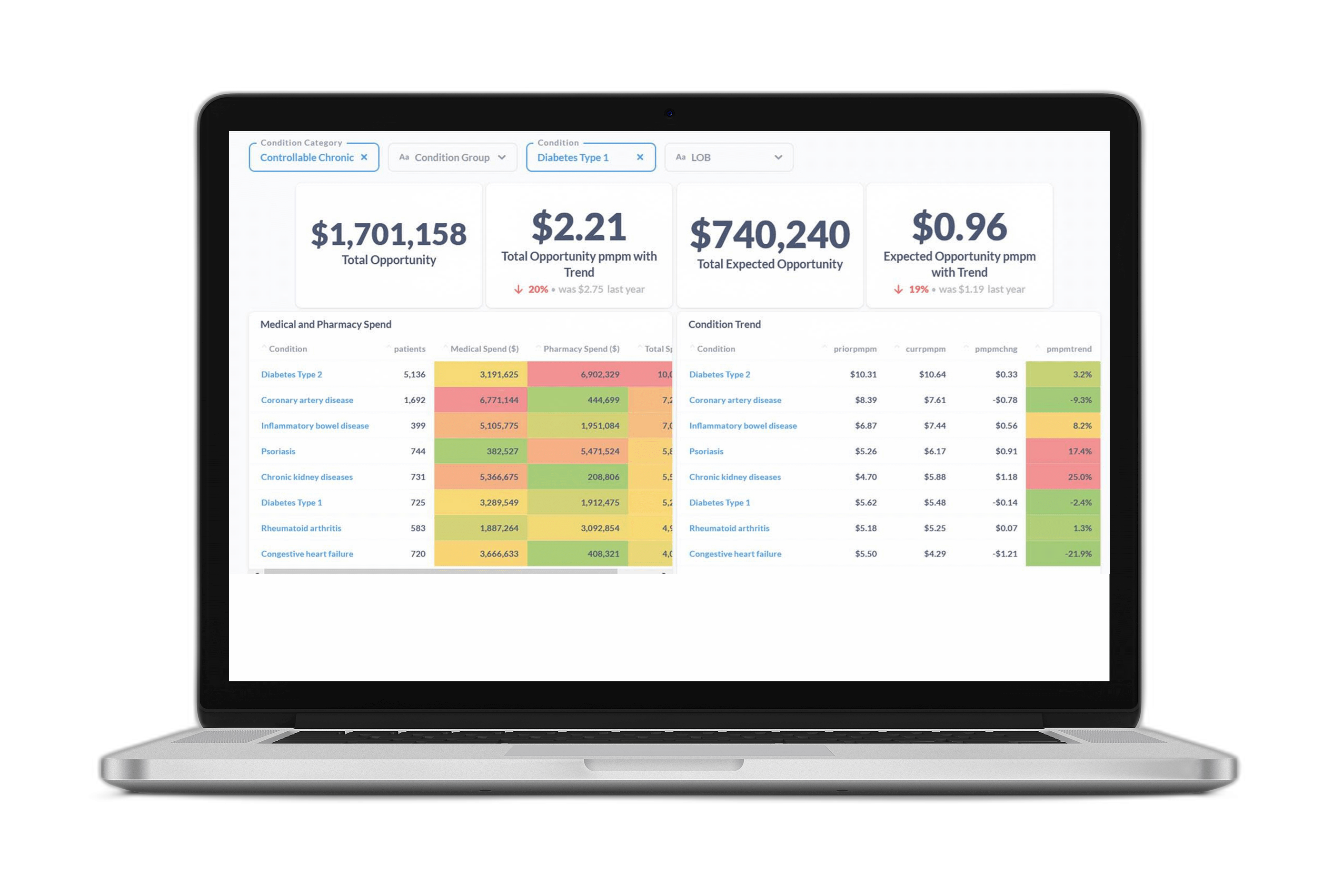
As healthcare organizations transition to value-based care, they’re moving toward prospective reporting that predicts not just risk, but modifiable risk, as we do through the Certilytics Opportunity Framework. This is the best way to reach members before they incur avoidable, exorbitant costs—and unlock true value while improving population health.
Thanks again to all those who made time to connect with us in Boston—we hope to connect again (or for the first time) at HLTH 2022!
For a free product demonstration or consultation with our team of experts, reach out to us at contact@certilytics.com