Shift to member-focused programs using Certilytics library of 1,000+ clinical, financial and behavioral predictive risk scores to identify future risks and opportunities at the individual level.
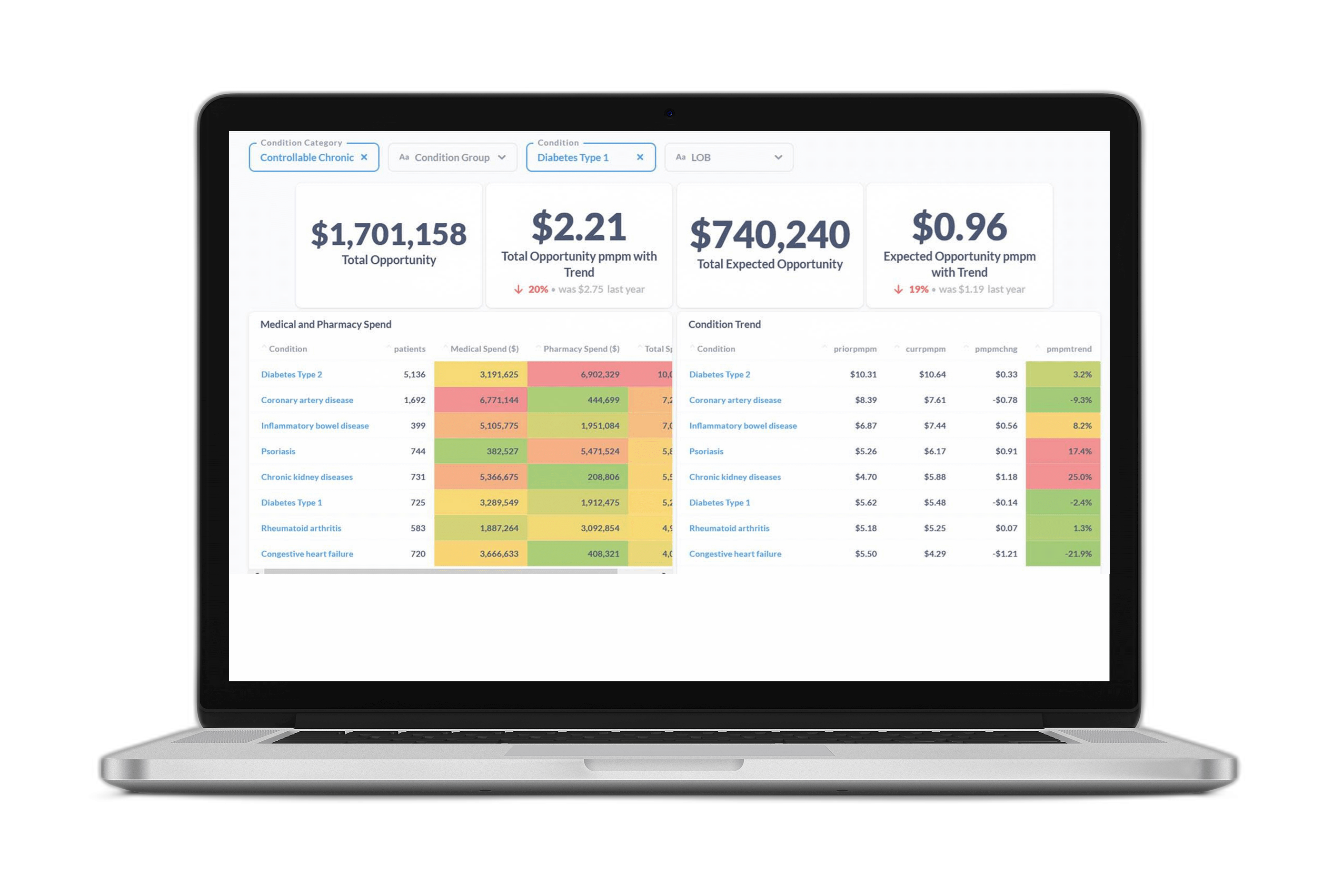
Aggregate member level opportunities up to the population level using the Opportunity Analyzer and see in dollars the impact of executing different clinical programs based on outcomes or disease state.
Be confident your clinical program outreach strategies are reaching those members who are most likely to modify their behavior and improve their health using Certilytics’ member-level Target Index. This approach allows you to maximize your outreach and streamline operational and clinical resource efficiency.